Health Workforce Planning Through Complexity: Tackling Multiple Problems in Tandem Within Complex Adaptive Systems
Health workforce planning is riddled with challenges. When we gather in large-scale meetings, it’s common to spend hours unpacking the many issues we face. But that wasn’t the approach taken at the WHO’s Looking to the Future: Modelling and Optimizing the Health and Care Workforce (April 27–30) in Copenhagen. Instead, we were invited to begin by rethinking our assumptions.
Interconnected systems
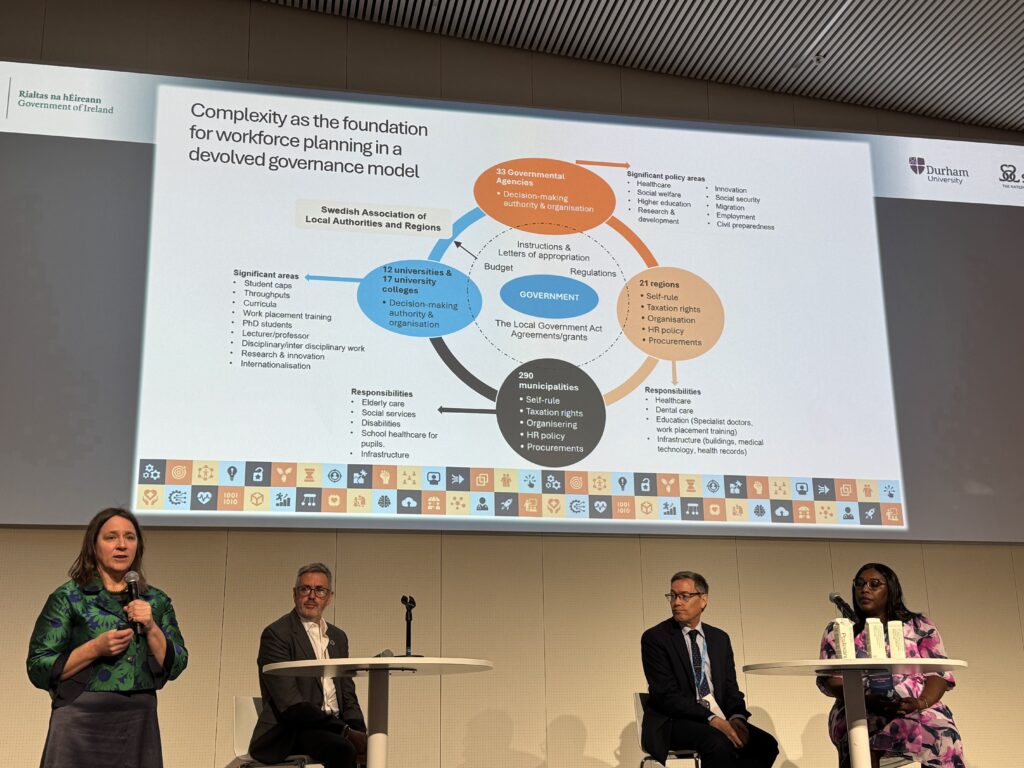
Dr. Brian Castellani, Director of the Durham Research Methods Centre in the UK, opened the event with a compelling plenary on the importance of embracing complexity in adaptive systems. He reminded us that the health human resources “problem” is a wicked one. In reality, health workforce planning is a web of many interconnected and entangled challenges: workforce shortages, retention, safe working conditions, education and upskilling, recruitment (both international and domestic), and more.
But these health workforce planning challenges don’t exist in isolation. They are nested within broader health system complexities, which themselves are embedded in even larger political, economic, and labor market systems. In essence, health workforce planning is a complex system within systems within systems.
To illustrate this, Brian showed a slide filled with chaotic, multicolored scribbles. At the centre was a simple black box with stick figures trying to solve a single problem using a single straight arrow. The message was clear: focusing on one issue while ignoring the surrounding complexity is unlikely to yield meaningful results.
Instead, we must embrace complexity and use it as a strength. That means welcoming diverse perspectives and new ways of thinking. It means not shying away from the big picture when setting a bold new vision for the future. And it means designing solutions that pull multiple levers at once—solutions that are resilient, adaptive, and built to last.
Of course, the notion of system complexity can feel daunting—perhaps even overwhelming. Why not just chip away at the health workforce planning iceberg one ice cube at a time? The answer lies in a phenomenon called “regression to the mean.” While statistical in origin, this concept applies broadly to human systems. It reminds us that even when we push for change, the adaptive systems we operate within often pull us back toward the status quo. It’s the essence of the old adage: the more things change, the more they stay the same.
“Back-casting” to move forward
Building on this, Dr. Gareth Rees of Universidad ESAN in Peru introduced the concept of “back-casting”—a health human resources planning approach that places system complexity at its core. Unlike traditional forecasting, which starts with the present and builds forward, back-casting begins with a bold vision for the future and works backward to identify the steps needed to get there. Gareth argued that forecasting often embeds the flaws of the current system into future plans, limiting transformative potential.
Back-casting, by contrast, involves two key steps: first, bringing together diverse stakeholders to define a desired future state; and second, assessing the gap between that vision and the likely future based on today’s trajectory. The second step focuses on the “how”—developing multi-level, multi-sectoral strategies to drive long-term system transformation. [See footnote 1 for a webinar link on this topic you might find useful.]
A Swedish use case
Several countries are already seeing success with this approach. For example, Asa Olsen, Health Workforce Specialist with the Swedish National Board of Health and Welfare, shared early results from pilot projects using a modified back-casting model. These projects focus on embracing digital in health workforce planning, optimizing work environments, aligning workforce planning with education, and more. The Swedish ‘back-casting’ approach includes four iterative steps:
- Setting a concrete, targeted vision
- Co-designing multi-pronged solutions with system actors
- Embedding learnings into current systems
- Regularly reassessing progress
Asa emphasized that this work requires focused leadership and a commitment to sustainable change. [See footnote 2 for a webinar link on this topic you might find useful.]
Embracing complexity
What became clear during the WHO event is that embracing system complexity and using innovative planning approaches cannot succeed without collaboration. No single organization, country, or planner can do it alone. We must align on a shared vision. We must understand our roles. We must act—and be willing to adjust course as we go.
Embracing complexity isn’t a solution in itself. It’s a mindset. A way of reframing how we approach the health workforce planning challenges of today. And while it can feel overwhelming, it’s also empowering. It reminds me that we each have a role to play. That our collective efforts matter. And that together, we can shape a better future.
I look forward to continuing this work with the WHO and the many countries that came together in April—and to exploring how back-casting within complex adaptive systems might be applied in the Canadian context.
Footnotes:
- Gareth Rees and Cris Scotter Introducing Backcasting for Health Workforce Planning
- Asa Olsen Swedish National Board of Health and Welfare Bing Videos

Insights and reflections from Deb Cohen, COO, Health Workforce Canada
